Total hip replacement (THR) is one of the most successful surgical operations in terms of increasing quality of life. In a hip replacement, the arthritic surfaces of a damaged hip are replaced with artificial components called a hip prosthesis.
After a long history of efforts to develop a lasting artificial hip it was Sir John Charnley, in Wrightington UK, who introduced the first effective hip replacement in 1962. Since then a large number of designs have been introduced, with very good long-term results in some prostheses such as the Exeter Hip.
According to the National Joint Registry of the UK there were over 88,000 primary hip replacements and over 9,500 revision procedures in 2014. Of the primary hips, 31% were cemented total hip replacements (THR) and 41% were cementless THRs. 27% were hybrid procedures and around 1% were hip resurfacing.
Trends are moving away from hip resurfacing and cementless THR and towards hybrid procedures. Hybrid procedures mean that one component is cemented and one is not.
Hip Anatomy
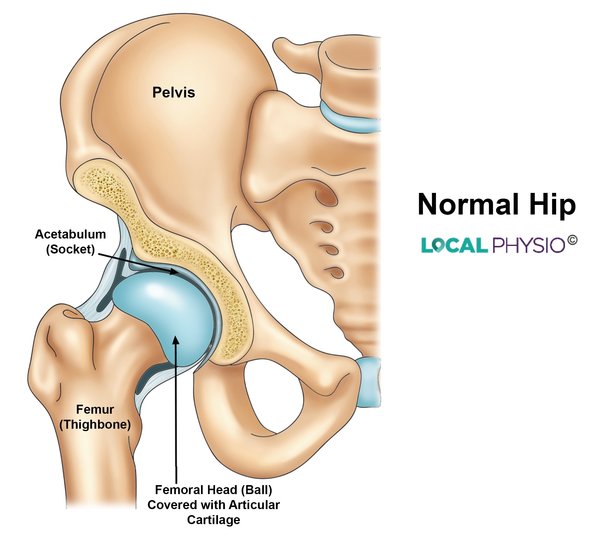
The hip is one of the largest joints in the body and classified as a ball and socket joint. The head of the femur is the ball, an almost spherical shape covered with a layer of slippery articular cartilage.
The socket, called the acetabulum, is deep and is again lined with articular cartilage. The socket is made deeper by a rim made of fibrocartilage known as the hip labrum which runs all round the socket.
The hip joint has large and powerful ligaments holding it together for when we do vigorous things like running or jumping. For this reason dislocation of the hip is uncommon without significant force such as a car accident.
The hip joint also has the body’s largest and most powerful muscles acting on it, the buttock muscles. The main ones are gluteus maximus, gluteus medius and gluteus minimus.
The hip is a weight-bearing joint and is designed to cope with activities such as walking, running, jumping and lifting weights.
Why Have A Hip Replacement?
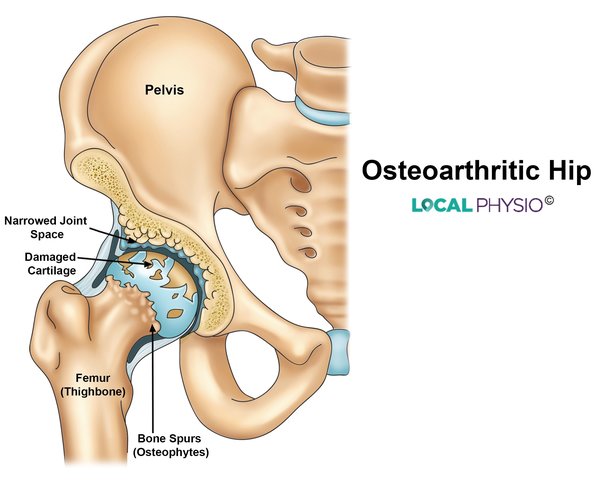
A hip replacement is a major operation with potential side effects that can be important. The hip problem should be severe enough for the benefits to outweigh the risks of operation.
Reasons to have a hip replacement include:
- True hip pain
- Pain significantly gets in the way of normal life such as getting dressed and driving
- Sleep is disturbed by the pain
- Walking distances are gradually reducing
- Hip movements may be lost
- The x-ray shows a fracture, rheumatoid arthritis or osteoarthritis joint changes
A hip replacement is designed to relieve pain, improve mobility and quality of life and restore normal day-to-day activities. It is not designed to take large forces such as in running, skiing, squash or contact sports.
You can check the record of surgeons in your area specialising in joint replacement (UK only) by visiting NJR: www.njrsurgeonhospitalprofile.org.uk
Who Has A Hip Replacement?
Total hip replacement is overwhelmingly performed for older people between 60 and 80 years of age, although both younger and older people do have a successful hip replacement.
In 2014 the average was just over 68 years of age with 60% of patients being female. The highest percentage of patients was in the 70-79 year age group. Patients having resurfacing procedures had a younger average age at 54 years.
Types of Hip Replacement
Metal on Plastic designs
The initial design by John Charnley was a metal-on-plastic design, with a metal ball and a plastic socket. This design has been developed and tested for the longest.
Modern designs use stainless steel alloys for the stem and head and ultra-high molecular weight polyethylene plastic (UHMWPE) for the socket. This ensures very low wear between the two types of surface (around 0.1mm a year) and an easy friction-free movement of the joint.
Metal on Metal Designs
Metal on metal designs have been tried since the 1950s and may offer low wear and less bone loss from particle debris compared to plastic sockets.
Larger femoral heads, mirroring the true size of the femoral head, can also be used, which may reduce the risk of dislocation. Wear products in this type of hip are metal ions and although these do travel around the body they have not been shown to cause harm.
Ceramic Designs
Ceramic materials are very hard and durable, wear very little and don’t cause any toxic effects within the body. Hip replacement implants can be ceramic on ceramic or ceramic on polyethylene.
- Ceramic on ceramic (CoC) designs combine good reliability with good long-term results. These hips are often used in younger or very active patients. Wear levels are very small indeed, meaning the complications of bone loss and inflammation from wear particles can be avoided.
- Ceramic on plastic implants also have good wear properties due to the ceramic head having an ultra-smooth surface.
Hip Resurfacing
In a standard hip replacement, a significant amount of bone is removed from the upper femur. To try and avoid this, the technique of hip resurfacing was developed, where an artificial cap is put on the ball of the hip, retaining the greater part of the femoral head.
Hip resurfacing has not yet been shown to be a more reliable method of hip replacement or to give better function over time and remains in a minority of hip replacements performed.
Cemented or Uncemented?
Apart from the implant material and designs, hips can be inserted with or without cement:
Cemented hips. This is the original technique with metal on plastic hips, the cement is used to fill in the gap between the bone and the prosthesis. It allows a mechanical interlock to be formed which is the basis for the long-term stability and durability of the joint.
Uncemented hips. In this technique, the components are press-fitted into a shaped bony space created by the surgeon. Uncemented components may have surfaces with mechanical or chemical coatings to encourage bone growth up to and through the prosthesis to achieve stability.
Overall there may be only small differences in “implant survival” between the two groups, meaning that the hip remains in place and is functioning well.
Cemented hips may have better short-term results and over the long term have better results in the 65 years and older group. In patients from 55 to 64 years old there is no clear difference.
Physiotherapy For Hip Osteoarthritis
Physiotherapy for an OA hip starts long before anyone is considered for hip replacement. A physio can help with:
- Strengthening the buttock and thigh muscles
- Teaching a normal gait pattern
- Maintaining the ranges of hip movements
- Teaching the correct use of a walking aid
- Pacing activity
- Encouraging weight loss.
Self-management of an arthritic hip is very important and can delay or in some cases remove the need for a hip replacement operation. Physiotherapy can also help prepare someone for a hip replacement by keeping up muscle strength, joint movement and as normal a gait as possible.
Physiotherapy After Hip Replacement
After your operation staff from the physiotherapy department will get you up, help you to walk and teach you the appropriate way to get in and out of bed. This will likely be on the first day after your operation but could be the second day, depending on your medical condition.
In the past patients were taught to take careful precautions with hip movements to avoid dislocation but more recent work has shown this not to be helpful.
Physiotherapists teach normal gait patterns, the use of crutches, how to progress off walking aids, how to return the hip to full movement and how to strengthen the hip muscles. Once a person understands their rehabilitation and returns to normal activities, further physio is usually unnecessary.
Results Of Total Hip Replacement
Hip replacements are now expected to last at least 15 years if there are no complications and recent research shows that many may last up to 25 years. People have reported good functional outcomes up to and beyond 16 years since their replacement.
Survival rates at ten years are over 90% in most studies of well-researched systems such as the Exeter hip, meaning the hip replacement remains in place without significant problems.
Revision Hip Replacement
Up to 10% of hip replacements have to be redone at some point over ten years. The most common problem is known as aseptic loosening, loosening which occurs in the absence of infection. The most serious problem is an infection as this is difficult to eradicate.
The revision hip replacement operation is more time-consuming and technically demanding than a primary hip replacement. Some surgeons specialise in these operations and the post-operative recovery can be slower due to limitations on the amount of weight-bearing allowed.
References:
- National Joint Registry NJR Reports. http://www.njrreports.org.uk/
- NJR Surgeon and Hospital Profile. http://www.njrsurgeonhospitalprofile.org.uk/
- Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. Mäkelä KT et al. BMJ 2014;348:f7592. http://www.bmj.com/content/348/bmj.f7592
- How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Evans JT el al. The Lancet 2019: vol 393, issue 10172, p647-654.
Last Review Date: 08-12-2019
Next Review Date: 08-12-2021