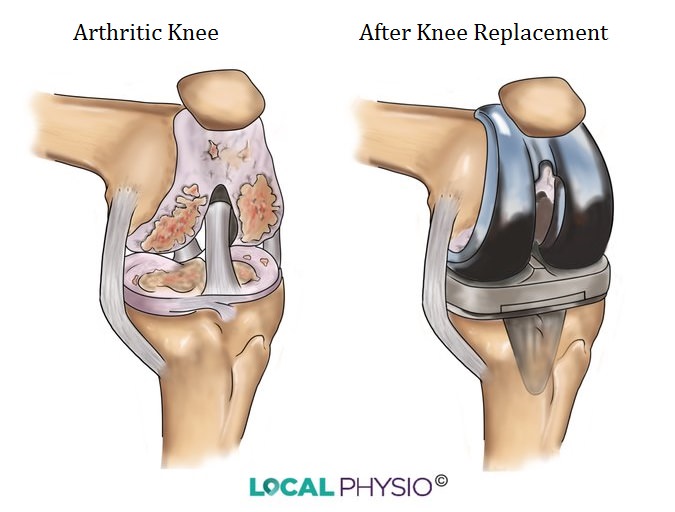
Total knee replacement (TKR), or total knee arthroplasty (TKA), is the replacement of the arthritic joint surfaces of the knee with artificial components.
Although not as successful initially as the early hip replacements pioneered by Sir John Charnley in the UK, knee replacement has matured into a routine and predictable treatment for the severe knee pain of arthritis.
The modern success of knee replacement is based on advances in understanding the complex movements of the knee joint and the development of new approaches in the metals, plastics and ceramics used to manufacture the prostheses.
Around 97,000 people have knee replacement procedures every year in the UK and over 719,000 in the US.
Anatomy Of The Knee
The knee is a large hinge-type joint with a more complex movement than a simple hinge. Movement of the knee is a combination of bending, rolling and sliding as the knee bends and straightens.
The shape of the bones of the knee joint and the four major ligaments holding it together dictate the amount and types of movement that can occur.
- The lateral collateral ligament and the medial collateral ligament lie across the knee joint on the outside and the inside respectively. They hold the knee in place against side-to-side stresses.
- The cruciate ligaments hold the knee against front and back stresses and the anterior cruciate ligament is the one commonly ruptured in sport. The cruciates are also often removed during the knee replacement operation.
The Patellofemoral Joint
The joint between the knee-cap (patella) and the front of the thigh bone (femur) is the second and much smaller knee joint. The kneecap slides back and forth against the femur and can be affected by arthritis in the same way as the knee.
Who Should Consider Knee Replacement?
Knee replacement is a major operation and there can be side effects and long-term problems in some cases.
Reasons you may have a knee replacement are:
- Knee osteoarthritis or rheumatoid arthritis
- Disabling knee pain that interferes with normal activities
- Sleep disturbed by knee pain
- Walking may be very limited
- Joint deformity such as bow-leg or knock-knee
- Significant osteoarthritis on x-ray with loss of joint space
- Severe patellofemoral pain
Symptoms must be severe enough because joint replacements have a limited lifetime and this can be reduced if a high activity level is resumed after the operation. So knee replacement is more suitable for older people who wish simply to walk about, drive a car and manage stairs.
Knee replacement may be suitable for younger people with many joints involved due to arthritis throughout the body. In these patients their activity will be limited by their other joint problems.
Young people, with an arthritic knee due to knee injuries or a fracture, are not excluded from this operation and this age group is increasingly operated on. There are limitations on the use of a new joint in a young person. If they go back to vigorous activity the life of the new joint could be very short and re-doing the joint (revision) is much more complex.
A Knee Replacement Might Not Be Suitable If:
- Infection is present in the knee
- A significant infection is going on in some other part of the body
- The main thigh muscles are not functioning properly
- Blood supply to the leg is very poor
- The knee is fused straight and working well.
Other reasons to be cautious about a knee replacement are being medically unwell, a history of infection in the joint, a loose joint due to loss of nerve feeling and perhaps being significantly overweight.
Types of Knee Replacement
Many types of knee replacement have been developed to cater for the different types of problems people have with arthritic knees. Overall there is little to separate these designs in terms of outcome over time.
The most common brand types of knee replacement in the UK are the PFC Sigma Bicondylar Knee (at around 35%) with the Nexgen (15%), Triathlon (10%), Vanguard (<10%) and Genesis 2 (<10%).
Medical Checks Before The Operation
Patients must be able to cope with the anaesthetic, blood loss and rehabilitation so a thorough medical work up is done before admission, usually in a pre-admission clinic.
X-rays of the joint and chest, ECG to check heart function, urine and blood tests and consultations with medical experts may all be part of the examinations.
X-rays
X-rays of the knee are usually a front-to-back view and a side view and may be taken in standing. A special view, called a skyline view, may be taken to assess whether the patello-femoral (kneecap) joint is normal.
Typical signs of osteoarthritis on an x-ray include loss of the joint space (the bones appear closer together), increased density of the bone beneath the cartilage and bony outgrowths (osteophytes) at the margins of the joint.
The Anaesthetic
A general anaesthetic or regional anaesthetic may be used. Regional anaesthetics numb just the operated area and the patient remains conscious but sedated.
The long term outcomes and risks have not been shown to be any different between these two types of anaesthetic. The anaesthetist usually decides this in consultation with the patient, taking the medical history into account.
People who have a regional anaesthetic get on more quickly after operation and have fewer early complications.
Nerve blocks, such as a femoral nerve block, can be used to reduce pain post-operatively and have been found to be useful.
The Knee Replacement Operation
Knee replacement is performed in an operating room designed to minimise the chances of infection.
- The surgeon usually performs the operation from the front of the knee with the cut to the inner side of the patella.
- A tourniquet may be applied to the upper thigh.
- The arthritic bone surfaces are removed from the lower femur and upper tibia, using specialist jigs to ensure the amount and angles of the cuts are correct.
- The amounts of bone removed are calibrated so the line of the knee joint is at its normal position once the new joint is inserted.
- Any ligament over-tightness is released to allow normal movement after the operation.
- Trial components are inserted and the knee is bent and straightened to make sure the kneecap is tracking along the right lines.
- The tracking of the kneecap against the thighbone is carefully assessed. If it is running too far to the outside, the tissues on that side may be cut and tissues on the inside may be tightened up. This can make recovery slower as there is more tissue damage and pain involved.
- The new joint components are cemented into place, including a plastic button to the back of the kneecap if that is required.
- If uncemented components are used, these are press-fitted.
- The tourniquet is released and the wound checked before it is stitched. A pressure bandage is applied to reduce swelling and bleeding. A plastic drain is placed in the wound and drains out into a bag on the side of the bed to prevent build up of fluid or blood in the wound.
- Injection of local anaesthetic around and into the joint during surgery gives good pain control with reduced morphine intake and increased progress after operation.
The Post-Operative Period

The initial few hours after operation are spent in a recovery or high-dependency area until the patient is stable enough to be transferred back to the ward. Painkillers are administered by epidural, patient controlled analgesia or orally. Cold therapy may be used to reduce swelling and pain.
Knee movements start the next day under the supervision of the physiotherapist and sometimes a continuous passive motion (CPM) machine may be used. Getting going early is beneficial and leads to early discharge.
The drains usually come out at 24 hours unless they are draining a lot. Walking with the physiotherapist begins on the first or second post-operative day, with elbow crutches or a frame depending on age or ability.
Discharge
Discharge often occurs when the wound has healed sufficiently, pain is under control, knee bend is 90 degrees or close to it and the patient is able to manage daily tasks and walking. First follow up by the doctor is typically at six to twelve weeks after surgery.
Physiotherapy after discharge can be very useful to increase joint range, increase muscle strength, improve balance and encourage a return to normal activities.
Long-term Follow Up
This depends on the local health care system and the requirements of the surgeon. Typical follow up times might be at six weeks, three months, six months, a year, two years, five years, ten years and then as required. This follow up will vary with the medical status, age, complications and level of activity of the patient.
The Outcome Of Knee Replacement
Most people are pleased with the results of their TKR. They can manage normal activities of daily living and low level sporting activities. It is not wise to play higher-level sports with a knee replacement, as this may shorten the life of the new joint.
Scientific studies have shown good function in knee replacements in around 90-96% of patients at 15 years after operation. It does not seem to make any difference if the cruciate ligaments were removed at operation or not. Knee replacements which do not use cement (cementless designs) are showing good results although they have not yet been studied for the same length of time.
Recent research in The Lancet has indicated that 82% of total knee replacements and 70% of unilateral knee replacements last 25 years in patients with osteoarthritis, so if you have a replacement, you have a good chance of it surviving longer than you do. The average age for knee replacement is around 70 years.
References:
- Knee Replacement. NHS Choices. http://www.nhs.uk/conditions/Knee-replacement/Pages/Kneereplacementexplained.aspx
- Knee replacement surgery. Arthritis Research UK. http://www.arthritisresearchuk.org/arthritis-information/surgery/knee-replacement.aspx
- National Joint Registry http://www.njrreports.org.uk/
How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Evans JT et al. The Lancet 2019: vol. 393, issue 10172, p.655-663,
Post op image courtesy of olovedog at FreeDigitalPhotos.net
Last Review Date: 08-12-2019
Next Review Date: 08-12-2021