Osteoarthritis or OA is the most common joint condition in the world, affecting hundreds of millions of people. It is responsible for the largest amount of disability of any medical condition. Physiotherapy is extremely helpful in managing the long-term effects of osteoarthritis.
A Normal Joint
Where two or more bones meet together is a joint. Our bodies have large numbers of different kinds of joints but the most common are called synovial joints. These include all our major mobility joints such as hip, knee, shoulder and ankle.
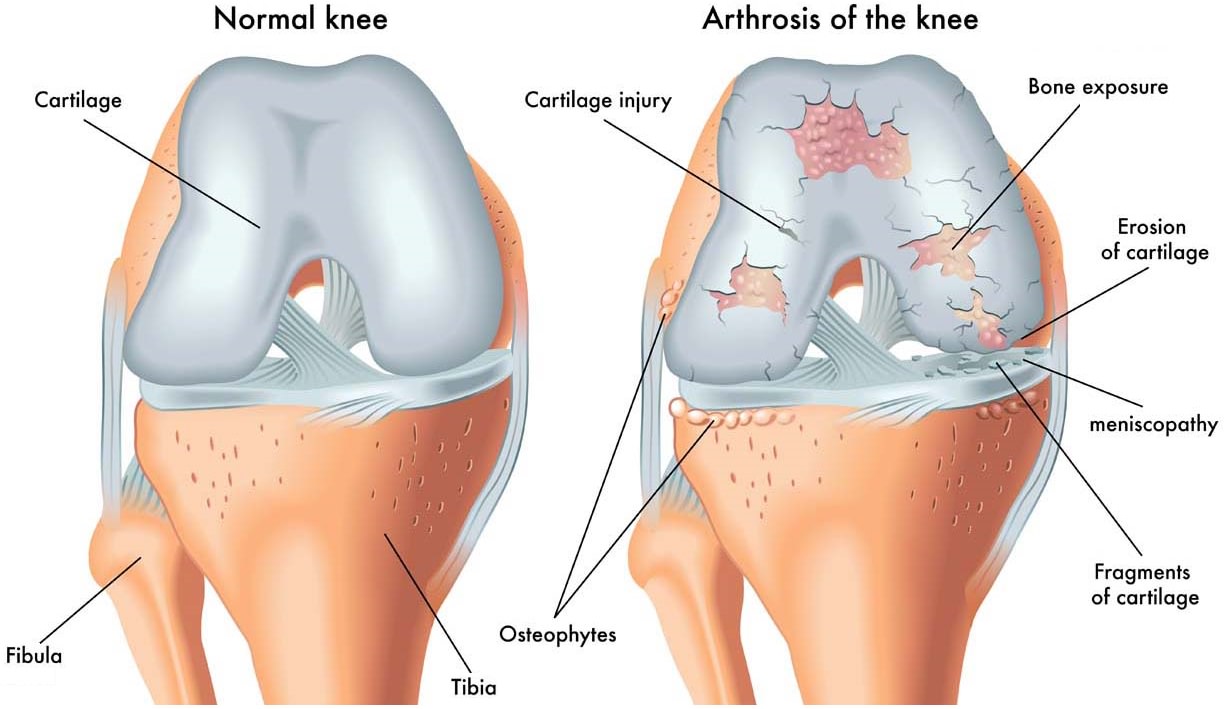
The surfaces of these joints are covered by articular cartilage, a firm, slippery material about 3mm or 1/8th of an inch thick. This allows painless and effortless movement of the joint even under load. A small amount of fluid is present and aids movement.
What is Osteoarthritis?
Osteoarthritis is a joint condition which changes the way the joint works and feels so it no longer moves smoothly in the background. A number of terms are used to describe osteoarthritis including degenerative joint disease, wear and tear, arthrosis and ostoearthrosis. They all refer to the same process now called osteoarthritis. Modern thinking is that many of the joint tissues are involved in the process and not just the cartilage.
When Osteoarthritis develops these changes occur:
- The smooth articular cartilage thins out and roughens as it develops small cracks and flakes.
- The bone underneath the cartilage becomes denser.
- The lining of the joint which produces synovial fluid may start to produce more than normal and cause swelling in the joint.
- The joint tissues become more active to try and repair the ongoing damage so the joint may feel warmer than normal
In more severe cases:
- Severe loss of the cartilage layer may allow the bones to rub and grate together. This can be heard as an audible crunching.
- Lumps can form as the bone around the joint grows outwards, making bony spurs known as osteophytes.
- The surrounding ligaments and joint capsule, designed to keep the joint stable, may thicken up and shorten. This limits the movement of the joint and may be the body’s reaction to a potentially unstable joint.
- Knock-knee or bow-leg may develop as the areas suffering the greatest loads also incur the worst arthritis changes.
These changes may result in pain, loss of movement and loss of muscle power.
Osteoarthritis Symptoms
The most common symptoms of osteoarthritis are:
- Pain. This is the main reason people go to the doctor. Mild stiffness and aching after heavy use will occur first in most people, progressing to a deep ache on activity. This may worsen until the joint is painful at rest or at night and very troublesome on movement or weight bearing.
- Stiffness. The joint will feel stiff on getting going so it will be very stiff in the morning but will ease within 30 minutes. The joint may stiffen or “gel” after resting for a period following exercise or activity.
- Grinding or grating feelings or noises, known as crepitus, are very common. Crunching and creaking can both be felt and heard in severe cases.
- Swelling. There are two types. One is the hard bony swelling of the joint caused by extra bone formation and the second is the extra fluid inside the joint.
- Wasting of the main quadriceps muscles may be evident.
- Loss of joint function. The joint may have restricted movement, loss of power and feel unstable.
An osteoarthritic joint can vary from day to day and be worse or better for no obvious reason, perhaps in response to changes in the weather.
What Causes Osteoarthritis?
It is not clear what the cause of OA is but it is likely to be a mixture of genetic and life factors such as:
- Age. The incidence of OA increases for every decade of life and it is estimated to occur on x-rays of 80-90% of people over 65. By 80 years of age everyone has some affected joints. Many people have no symptoms from their OA joints. Most people are over 50 before they have any symptoms, perhaps due to the chemical changes in cartilage and a reduced supply of nutrients.
- Gender. OA is more severe and more common in women, especially OA of the hand joints and the knees.
- Injury. An injury to a joint which changes the smooth surface or the angle of the joint can result in abnormal loads speeding up the degenerative process. Some very demanding jobs, such as farming, increase the chances of getting OA.
- Repeated small joint insults may add up over time to damage a joint. This can occur in activities or jobs where frequent kneeling, stair climbing or squatting is involved.
- Obesity. Being overweight is related to developing osteoarthritis and it may contribute to worsening of the joint changes over time. This is particularly relevant to knees and may also be important in hips.
- Abnormalities of joints. Any joint abnormality may increase the likelihood of developing OA. Examples are DDH or development dysplasia of the hip, where the hip ball and socket fail to form normally and become arthritic in adulthood. There is a suspicion that most OA in hips or knees may be due to unrecognised defects in or damage to the joint.
- Surgery and trauma. Repair of the cartilage, ligaments and menisci (the small spacers in the knee) can restore normal function to a joint, but around 50-60% of patients develop osteoarthritis to some degree from five to fifteen years later.
- Genetics. The only clear genetic link is for what’s called nodal osteoarthritis, which affects the small hand joints in older women and runs in families.
- Inflammatory arthritis. OA may develop as a secondary consequence of joint damage from rheumatoid arthritis, gout or other arthritic conditions.
Which Joints Get Osteoarthritis?
While osteoarthritis can occur in any joint due to injury or abnormality it is much more common in certain joints, particularly weight bearing ones. It is often symmetrical, occurring to some degree in joints on both sides.
- Knees. Common in older people, especially women. If severe may lead to total knee replacement.
- Hips. Again common in older people and may require total hip replacement.
- Spinal. The small joints in the back and neck (not the major disc joints) can become arthritic and give stiffness, pain and limited movement.
- Hands. The small hand joints may develop bony swelling, become stiff and go off at angles to straight. The most common and troublesome is the joint at the base of the thumb.
- Big Toe. This joint is susceptible to changes in the same way as the base of the thumb.
Complications of Osteoarthritis
There are two joint conditions which are more likely to occur in people with Osteoarthritis:
- Gout. This is an inflammatory arthritis and is more common than realised. Higher levels of the chemical urate in the blood can lead to crystals being formed in and around a joint. This is more likely if the person already has OA. The big toe joint is the most common site for this disease and also a common place for OA to occur.
- Chondrocalcinosis. Crystals of a material called calcium pyrophosphate may form in a joint. This can occur without OA but is more common in older people with OA of the knee. This may speed up the worsening of OA and in some cases the crystals can bring on an acute arthritis. This causes a severely painful, hot and swollen joint and is termed acute CPP or acute calcium pyrophosphate crystal arthritis.
Diagnosing Osteoarthritis
There are over 100 different types of arthritis so it’s very important to see a doctor for the correct diagnosis before planning the management. Treatments for different types of arthritis vary greatly so the appropriate treatment must be chosen.
Diagnosis of Osteoarthritis is done by noting the signs and symptoms:
- Pain on movement
- Tenderness on handling the joint
- Crunching and creaking on movement
- Hard swelling around the joint
- Fluid swelling in the joint
- Limited range of movement
- Abnormal movement and joint laxity
- Loss of muscle size and strength
A doctor may ask for tests:
- X-rays. With most osteoarthritis joints this is not necessary as the diagnosis will be clear. However it can show the state of the joint to compare against future x-rays to monitor the progress of the condition. The amount of joint damage on x-rays is not well linked to how much pain or problems people have.
- MRI scanning. This is more suitable for looking at soft tissues such as the menisci, cartilage, ligaments, muscles and tendons. It can indicate problems with these which may need intervention.
- Blood tests. These are not useful in osteoarthritis but if the diagnosis is uncertain they may point to a different kind of arthritis.
The Prognosis For Osteoarthritis – How It’s Going To Go
We can’t tell how osteoarthritis will progress in any one individual. It may come on quickly and become severe within only a few years as joint damage develops. This may progress to deformity such as knock-knee or bow leg and become disabling.
More common is a slow process over a number of years without sudden worsening or changes in the function of the joint. This type of osteoarthritis is less likely to end up with a severely damaged joint.
The symptoms may wax and wane, or develop up to a worst point and then improve or change very little. Osteoarthritis is limited to the joints so there are no effects on other parts of the body as in inflammatory conditions such as rheumatoid arthritis.
Factors which point to a faster worsening of knee osteoarthritis are being older, being overweight, having knock-knee and many joints involved.
Osteoarthritis Treatment
The aim of treatment for osteoarthritis is to reduce the pain and encourage normal joint movement and function. Osteoarthritis cannot be cured except by joint replacement and the non-surgical management of this condition consists of:
- Patient Education – It is very important that patients understand what OA is, how it may change with time and how it differs from inflammatory diseases such as rheumatoid arthritis. Weight loss and exercise can have significant benefits and patients can learn good strategies for pain control and improving the function of their joint.
- Heat and Cold – Ice or heat may be used, with care for the health of the skin an important issue. Individuals usually find out which one suits them.
- Weight Loss – The less weight the body has to bear the less stress on the joints and the easier it is to move about.
- Exercise – General exercise such as bicycling and swimming can maintain overall fitness without excessive weight-bearing stress. Specific exercises to maintain muscle strength of particular joints has been shown to be useful.
- Physiotherapy – A physiotherapist can help with many of the treatments and management strategies mentioned here.
- Occupational Therapy – An OT takes a functional approach to managing activities of daily living by changing behaviours and suggesting aids and appliances.
- Joint Unloading – Using a stick or crutches can reduce the load on a hip or a knee and allow good mobility without so much pain.
- Drug Treatments – Doctors prescribe a number of pain relieving drugs for OA, very similarly to other sorts of pain. They start with paracetamol, add anti-inflammatory drugs if medically appropriate and may progress to codeine based drugs. Topical anti-inflammatories, creams that are applied to the skin, may be useful. Always take a doctor’s advice before starting any drug treatment.
- Joint Injections – Corticosteroid can be injected into the joint but the scientific evidence of its usefulness is not clear. Viscosupplementation is the injection of a material similar to natural synovial fluid in an attempt to improve a joint’s function.
- Surgery – If conservative treatment is not successful then a consultation with an orthopaedic surgeon may be useful. Arthroscopy may be used to trim worn structures within the joint. Osteotomy can re-align the leg and fusion can stiffen a joint and allow a stable, painless joint.
- Joint Replacement – Knee replacement and hip replacement are very successful procedures and both have a success rate of over 90%. On average they have to be re-done after ten to fifteen years which is usually a much more complex process. Younger people are having more joint replacements but will need to have their new joints re-done more than once.
Physiotherapy and Osteoarthritis
Physiotherapy is the main management for osteoarthritis once it is diagnosed and a joint replacement is not planned. A physiotherapist can help with:
- Increasing muscle strength
- Correct use of sticks or crutches
- Improving walking ability and technique
- Reducing pain with paced activity and the use of hot or cold
- Maintaining and increasing joint ranges of movement
- Unloading a joint with braces or splints
- Managing stairs and general mobility
Physiotherapists can perform a comprehensive assessment of a person’s abilities when they are osteoarthritic. This allows a detailed treatment plan for the long-term management of the condition.
References:
- Osteoarthritis – Arthritis Research UK:
http://www.arthritisresearchuk.org/arthritis-information/conditions/osteoarthritis.aspx - Osteoarthritis. Medscape – Author: Carlos J Lozada, MD; Chief Editor: Herbert S Diamond, MD | Mar 27, 2015
http://emedicine.medscape.com/article/330487-overview - Osteoarthritis – NHS – Introduction | 27/04/2015
http://www.nhs.uk/conditions/osteoarthritis/Pages/Introduction.aspx
Last Review Date: 27-09-2017
Next Review Date: 27-09-2019